Health tips after stroke
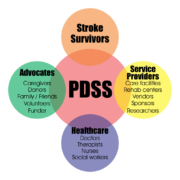
Life after stroke is difficult because there’s a change to your life but having the right support structure can help recovery process much smoother. this article will discuss Health tips after stroke.
At Coming Homme organization, we believe that stroke recovery tips should address both your physical health and your lifestyle, as both impact recovery.
Some of the Health tips after stroke includes:
Physical Healing Stroke Recovery Tips
- Understand How the Brain Heals
Did you know that the brain is capable of healing itself after an injury like a stroke? It revolves around the phenomenon of neuroplasticity: the mechanism that your brain uses to rewire itself and create new neural pathways.
- Focus on Good Nutrition
As your brain and body recover from the secondary effects of a stroke, you can boost recovery by focusing on proper nutrition. Some of the best foods for stroke recovery are whole foods like vegetables, nuts, and whole grains. It may also help to limit saturated fat and sugar intake.
- Don’t Get Discouraged If Progress Slows
You can’t mention Health tips after stroke without taking about the stroke recovery. At this point, recovery tends to slow down — but it will not stop as long as you don’t stop participating in rehabilitation.
Studies have shown that some stroke survivors are at the same level of improvement 5 years post-stroke as they were 2 months post-stroke. One possible reason for this long-term plateau could be a lack of consistent rehabilitation at home.
The brain needs consistent stimulation in order to rewire itself. To avoid getting stuck in a plateau, it’s imperative to find an appropriate home therapy regimen and stick with it.